Ticks & Tick-Borne Diseases
What are Ticks?
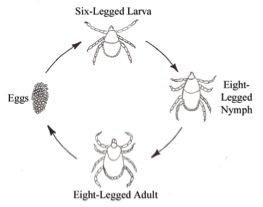
Ticks are external parasites (ectoparasites) that feed off the blood of mammals, birds, reptiles and amphibians. They belong to the class Arachnida as they have eight legs (the exception being the larval stage which has six) and are therefore not insects. They have four stages in their life cycle; egg, larva, nymph and adults. Individuals transition to each new life stage by moulting, following a blood feed. A number of tick species are vectors of human and animal diseases, as they can carry and transmit a range of viruses as well as haemoparasitic protozoans and bacteria.

Ixodes scapularis ex http://www.entm.purdue.edu/publichealth/insects/tick.html
There are two main groups of ticks; the ixodids or hard ticks (Ixodidae) and the argasids or soft ticks (Argasidae). The hard ticks have a hard dorsal shield (scutum). They are most commonly seen as they remain attached to their host for long periods of time. The soft ticks lack a hard scutum and feed only for a short time and are therefore seldom seen.
Globally 825 tick species are currently described, with 10 native species occuring in New Zealand. Most of them are bird (mainly sea birds) parasites (Carios carpensis, Ixodes kergulensis, I. amersoni, I. anatis (kiwi), I. eudyptidis, I. jacksoni, and I. uriae). But there are also the endemic tuatara tick (Amblyomma sphenodonti) as well as an undiscribed bat tick, and I. auritulus zealandicus which can also infest sealions. Only one species, the cattle tick (Haemaphysalis longicornis), is introduced and established. It has a wide range of mammal hosts, including humans.
Biology
Hard ticks and soft ticks have different life cycles. In general, the life cycle of a hard tick is as follows: A newly hatched (six-legged) larva feeds on a host, drops off to the ground, and moults to a nymph. A nymph seeks out and feeds on a second host, drops off to the ground, and moults to an adult. Hard ticks have only one nymphal stage, unlike soft ticks. Male and female adults seek out a third host, feed, mate and drop off to the ground. However, the number of host species utilised varies – there are also one-host ticks (eg. Rhipicephalus microplus) and two-host ticks (eg. Rhipicephalus evertsi). Males die soon thereafter, while females eventually lay eggs on the soil for several days to a few weeks. Depending on the species, a single female may lay 3,000 - 8,000 eggs and then dies without reattaching to a host again.
Hard tick life cycle ex http://www.napamosquito.org/Ticks/tick.htm
The duration of the life cycle differs depending on several factors, such as the type of hosts on which they feed or which developmental stage survives winter. For example, depending on the species, hard ticks may spend winter either as larvae, nymphs or female adults. A few species may have two or three developmental stages that over-winter. Some species complete a life cycle in as few as 90 days, others take a year, and a few require two years to complete a life cycle. In soft ticks, the life stages are not so easily distinguished and there is variation in the number of nymphal moults (up to 7). In general, the life cycle of a soft tick is as follows; eggs are laid in several batches of hundreds. Once hatched, the larvae require a blood meal from a host and moult to the first of their nymphal stages. They gradually increase in size with each moult until they reach the adult stage.Habitats and host seeking
Some of the most productive habitats of hard ticks are moist woodlands and areas of vegetation around the edge of forests, along forest trails, and in grassy fields. Hard ticks are more sensitive to desiccation than soft ticks and are usually found in environments which are protected from high temperatures, low humidity and constant winds. The type of hosts utilised varies between life stages of hard ticks. The most common hosts of larvae are small mammals, especially mice, and ground-dwelling birds and lizards. The hosts of the nymphs and the adults are medium sizes mammals such as pets, humans, deer or livestock. They generally use vegetation for host seeking and are often found in tall grass and shrubby areas. Adults commonly crawl up the vegetation and sit on the ends of leaves or blades of grass to seek out their host. Being flightless, hard ticks "wait" for passing vertebrate hosts. Larvae, nymphs and adults detect carbon dioxide, host odours, vibrations and warm moist air currents. They often can be seen at the tops of grass blades or on lower leaves of bushes engaging in "questing". Questing is a behaviour in which the tick reaches upward with waving front legs ahead of an approaching host. Tick larvae usually remain on the ground, where they encounter potential hosts. Nymphs remain on the ground or climb grassy vegetation from which they are able to grasp a passing host. Some soft ticks also quest for their host by climbing low lying vegetation.

Questing ticks ex http://www.ixodes-w5.org/icc.asp?oid=8557
The majority of soft tick species are nest parasites, which emerge only briefly to feed at night and hide during the day in or near the nest of the host. They are often found in burrows, caves, nearby rock crevices and nesting material. They remain hidden amongst the nesting material of their host while they are away and will rapidly move to feed on the host once it returns to the nest. Therefore not needing to actively seek hosts.
Soft ticks have high host and microhabitat specificity, most commonly associated with birds, particularly sea birds such as penguins. Some species are also parasitic on mammals including humans and occasionally bats.
Some species such as Otobius megnini (spinose ear tick) have adapted to a different life cycle. This species lives and feeds inside the ears of the host (naturally deer, mountain sheep and pronghorn antelope but now also cattle, domestic animals and humans), and employs a single host life cycle. The adult ticks do not feed and mating occurs on the ground. Many soft ticks thrive in hot and dry conditions.
Feeding
Hard ticks typically take one blood meal in each of the three developmental stages - larval, nymphal and adult. Both sexes are blood feeders, but only the female becomes greatly distended during engorgement. Hard ticks commonly feed on their host for long periods of time, sometimes as long as several weeks, with feeding time varying depending on life stage, species of tick and the type of host. Larvae of hard ticks usually complete a blood meal within a day or two and engorge very little. Nymphs attach to a host and complete a blood meal within a few days, they engorge enough so that red blood can be seen through their body wall. Male adults feed much like nymphs, but do so repeatedly on one host animal. They are only intermittent feeders and do not engorge as the large scutum greatly limits the amount that can be consumed at one time.
Females will not undergo feeding and engorgement until they have mated with a male tick. They attach to a host and feed to completion in a week or so. Engorgement is dramatic over the course of the last few days of feeding resulting in a huge increase in body size. Engorgement of female adults is facilitated by the lack of a large scutum and the possession of an expandable body wall. Fully engorged females of certain species may be over half an inch long and a quarter inch wide. The hard tick’s cuticle grows as the tick feeds to allow for the increasing amount of blood consumed.
Soft ticks will feed several times during each life stage and adult females will lay several small batches of eggs between each blood meal. Soft ticks usually feed rapidly and for only a short amount of time on their host, ranging from just several minutes to a few days. The cuticle of soft ticks expands as they feed but it doesn’t grow as in hard ticks, so they can’t consume nearly as much blood at one time. They may expand to anywhere from 5-10 times their unfed body size. Adults generally feed to repletion in minutes to hours, while larvae and nymphs feed for more extended periods. They usually have a longer life cycle than hard ticks, lasting through several years. Some soft tick species are also able to survive for long periods of time without feeding.
The act of blood feeding by a hard tick results in a "feeding wound." As it begins to feed, a tick secretes saliva containing compounds that increase blood flow, prevent clotting, and suppress the host's immune response. Ticks imbibe the blood that pools in the wound. At the same time, they regurgitate excess water that has been extracted from the blood meal into the wound. This process increases the possibility for the transmission of pathogens from a tick to its animal host.
Transmission of a pathogen typically does not occur until an infected tick has attached and fed for at least 24 hours, and transmission of some pathogens does not begin until an infected tick has fed for 48 hours or more.


Feeding tick and mouthparts ex http://www.medicinenet.com/rocky_mountain_spotted_fever_pictures_slideshow/article.htm
Diseases
Ticks are excellent vectors for disease transmission being second only to mosquitoes as vectors of human disease, both infectious and toxic. Ticks can transmit a wide variety of pathogens, including bacteria, protozoans and viruses to humans and animals. Some of the tick-borne diseases of greatest concern to human health include; Lyme disease, ehrlichiosis, babesiosis, rocky mountain spotted fever, tularemia, tick-borne encephalitis and tick-borne relapsing fever. Major animal diseases include babesiosis and anaplasmosis. Most tick-borne diseases are carried by hard ticks. Ticks can harbour more than one disease-causing agent, and therefore their hosts can be infected with more than one pathogen at the same time, compounding the difficulty in diagnosis and treatment.
Ticks are excellent vectors for disease transmission being second only to mosquitoes as vectors of human disease, both infectious and toxic. Ticks can transmit a wide variety of pathogens, including bacteria, protozoans and viruses to humans and animals. Some of the tick-borne diseases of greatest concern to human health include; Lyme disease, ehrlichiosis, babesiosis, rocky mountain spotted fever, tularemia, tick-borne encephalitis and tick-borne relapsing fever. Major animal diseases include babesiosis and anaplasmosis. Most tick-borne diseases are carried by hard ticks. Ticks can harbour more than one disease-causing agent, and therefore their hosts can be infected with more than one pathogen at the same time, compounding the difficulty in diagnosis and treatment.
Tick Personal Protection
- Wear light-coloured clothing with long pants tucked into socks to make ticks easier to detect and keep them on the outside of the clothes. Unfortunately, surveys show the majority of individuals never tuck their pants into their socks when entering tick-infested areas. It is unclear just how effective this prevention measure is without the addition of a repellent. Larval and nymphal ticks may penetrate a coarse weave sock. Do not wear open-toed shoes or sandals.
- Use of a DEET or permethrin-based mosquito and tick repellent can substantially increase the level of protection. This approach may be particularly useful when working in areas with a high risk of tick exposure.
- When walking keep to the centre of trails to minimize contact with adjacent vegetation.
- Unattached ticks brought in on clothing can potentially result in a later tick bite. Blacklegged ticks can survive for many days in the home depending upon the humidity. In the laboratory, nvmphal I. scapularis can survive for over 6 months at 93-100% relative humidity (RH). but over half will die in less than 4 days at 65% RH (RH in modern homes is generally <65%). On returning home. remove, wash and dry the clothing. Many blacklegged ticks and lone star ticks can survive a warm or hot water wash, but they cannot withstand one hour in a hot dryer.
- Carefully inspect the entire body and remove any attached ticks (see below). Ticks may feed anywhere on the body. Tick bites are usually painless and. consequently. most people will be unaware that they have an attached tick without a careful check. Also carefully inspect children and pets. A hypersensitivity reaction to tick bite may aid detection in a few individuals. but most people will be unaware a tick is attached and feeding.
Tick Control
The removal or regular maintenance of ground cover that provides shelter for ticks, cutting grass and removing covering shrubbery will assist in the control of tick populations.
Residual treatment of the ground cover in areas walked over regularly should remove some of the risk of individuals picking up ticks however ticks are able to detect and avoid pesticides. A barrier treatment of the populated area with a residual insecticide such as bifenthrin or permethrin, from the centre out, may provide good control.
Removing Ticks from Hosts
The safest and most effective way to remove an attached tick is to grasp it behind the mouthparts with fine forceps and pull gently and steadily away from the skin until the tick releases its hold. Do not twist, jerk or crush the tick's body as this may release body fluids harbouring pathogens, directly into the wound.Barbed mouthparts of the tick help to anchor it in the flesh of its host and ticks secrete compounds in their saliva that help to cement them in the feeding wound. Pulling too strongly or twisting while attempting to remove a tick may result in tearing of the tick, leaving the hypostome embedded in the skin. This can lead to bacterial infection in the feeding wound.
Do not attempt to remove an attached tick with caustic chemicals or by applying heat. This can kill the tick before it disengages its mouthparts. It can also cause the tick to regurgitate into the feeding wound and therefore increase the chance of transmitting a pathogen.

Tick removal ex http://www.medicinenet.com/rocky_mountain_spotted_fever_pictures_slideshow/article.htm
The removed tick should always be saved for identification, place into a sealed container and place in the freezer or add ethanol to the container. The attachment site of the tick should be washed thoroughly with warm soapy water and rubbing alcohol to remove any possible pathogens. Wash your hands as well as the tweezers or any other object the tick (or fluids from the tick) may have contacted. Objects used to remove or dispose of ticks as well as the site of the tick bite should be disinfected.
Tick-borne Diseases
Ticks are excellent vectors for disease transmission. They are second only to mosquitoes as vectors of human disease, both infectious and toxic. They can transmit a wide variety of pathogens, including bacteria, protozoans and viruses to humans and animals.
As our native ticks do not attach to humans, ticks would not be of any concern to human health in New Zealand if it was not for the introduced species of the cattle tick (Haemaphysalis longicornis) that is known to transmit theileriosis, babesiosis, tick-borne encephalites and several other diseases.
Every year there are interceptions at the border of other tick species (Heath and Hardwick, 2011), which can carry diseases of greatest concern to human health including Lyme disease, ehrlichiosis, babesiosis, rocky mountain spotted fever, tularemia, tick-borne encephalitis and tick-borne relapsing fever, as well as major animal diseases including babesiosis and anaplasmosis. Therefore personal protection and tick control is very important as is biosecurity and border control.
Lyme Disease
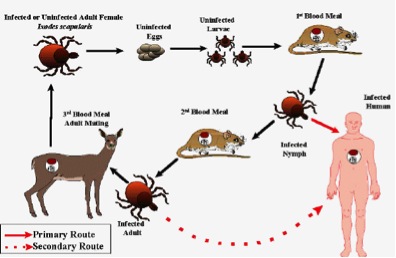
Lyme disease is caused by Borrelia burgdorferi, a bacterium carried by the blacklegged tick or deer tick (Ixodes scapularis), the western black legged tick I. pacificus and the sheep tick I. ricinus in Europe and by I. persulcatus in Asia. These ticks are usually found feeding on cattle, sheep, horses, dogs and cats.Lyme disease is endemic to North America and Eurasia. Symptoms include fever, headaches, fatigue and a distinctive “bullseye” rash on the skin (Erythema migrans). Infection can spread into the heart, joints and nervous system if it remains untreated.
Lyme disease can usually be confirmed through a blood test to detect the presence of antibodies designed to fight the disease. However, it takes six to eight weeks for the antibodies to show up, and so a blood test done soon after contracting the disease may be negative (falsely indicating absence of Lyme disease). Even after the disease has progressed and antibodies are present, the tests may sometimes still be negative when the disease is present (a "false negative" result). If there are signs of early symptoms, especially the telltale rash, immediate treatment is usually advised. As there is no certain cure for Lyme disease the blood test will continue to be positive for life, however it can be effectively treated with antibiotics. The earlier the disease is treated the better the prognosis for complete recovery. Successful treatment of the disease will not prevent contracting getting Lyme disease again. A Lyme disease vaccine is now available.

Erythema migrans rash ex
http://commons.wikimedia.org/wiki/Image:Erythema_migrans_-_erythematous_rash_in_Lyme_disease_-_PHIL_9875.jpg
http://commons.wikimedia.org/wiki/Image:Erythema_migrans_-_erythematous_rash_in_Lyme_disease_-_PHIL_9875.jpg
Rocky Mountain Spotted Fever (RMSF)
Rocky Mountain spotted fever (RMSF), like all rickettsial infections, is classified as a zoonosis. Zoonoses are diseases of animals that can be transmitted to humans. RMSF is caused by Rickettsia rickettsii, a bacteria that is transmitted to humans by the American dog tick (Dermacentor variabilis) and the Rocky Mountain wood tick (D. andersoni) in the United States, and Amblyomma cajennense in South America. Despite its name, RMSF is found in many areas outside of the Rockies, occurring throughout North, Central and South America.
These ticks are vectors and primary reservoirs for this bacterial pathogen. Mice, deer, grounding-feeding birds, wild rodents, and dogs are also reservoirs. Risk factors for contracting the disease are those who are frequently exposed to dogs and who live near wooded areas or regions with tall grass.
Symptoms of RMSF include sudden onset of fever, headache, and muscle pain, followed by the development of a rash. It can be difficult to diagnose in the early stages of the disease and can prove fatal if it is not treated. As the name implies, the illness presents with a very distinctive rash that indeed looks like spots.
The rickettsia are introduced into humans after an infected tick feeds for more than 6 hours. The tick bite is painless and frequently goes unnoticed.

Typical rash seen with RMSF ex http://www.physio-pedia.com/Rocky_Mountain_Spotted_Fever
Tick-borne Relapsing Fever (TBRF)
Tick-borne relapsing fever (TBRF) is caused by several species of spiral-shaped bacteria (Borrelia spp.) that are transmitted to humans through the bite of infected soft ticks of the Ornithodoros genus. Most cases occur in the summer months in mountainous areas of the Western United States. TBRF is a disease characterized by relapsing or recurring episodes of fever, often accompanied by headache, muscle and joint aches and nausea.Ehrlichiosis
Ehrlichiosis is a tick borne disease caused by several species of bacteria in the genus Ehrlichia, which are pathogens that cause disease in humans, dogs, cattle, sheep, goats, and horses. Currently, three species of Ehrlichia in the United States and one in Japan are known to cause disease in humans. There are three distinct ehrlichioses in the United States. The first is caused by the bacteria Ehrlichia chaffeensis, is transmitted by the lone star tick (Amblyomma americanum) which occurs in South eastern and southern central parts. Human granulocytic ehrlichiosis (HGE) represents the second recognized ehrlichial infection of humans in the United States. The name for the species that causes HGE has not been formally proposed, but is carried by the black legged tick (Ixodes scapularis) and the western blacklegged tick (Ixodes pacificus) in the United States.The third and most recently discovered ehrlichiosis is caused by Ehrlichia ewingii which has so far been limited to a few patients in Missouri, Oklahoma, and Tennessee. The full extent of the geographic range of this species, its vectors, and its role in human disease is currently under investigation.
Symptoms of Ehrlichiosis include headaches, myalgia, rigors and vomiting.
Sennetsu fever, caused by Ehrlichia sennetsu, in Japan is characterized by fever and swollen lymph nodes. This disease is very rare outside the Far East and Southeast Asia, and most cases have been reported from western Japan.
Canine ehrlichiosis is caused by Ehrlichia canis which is transmitted by the brown dog tick (Rhipicephalus sanguineus). Symptoms of canine ehrlichiosis include lameness and fever.
Proposed life cycle for the agent of Human Granulocytic Ehrlichiosis ex http://pathmicro.med.sc.edu/mayer/ehrlich-nh-hge.gif
Babesiosis
Babesiosis is an uncommon malaria-like parasitic disease caused by piroplasms, protozoan parasites of the genus Babesia. Babesia microti uses the same tick vector (Ixodes scapularis) as Lyme disease and HGE, and frequently occurs in conjunction with them. Babesiosis in humans is a rare potentially fatal disease, but is a common infection in animals. People can be infected with both babesiosis and Lyme disease at the same time.Babesiosis occurs in the north east of the United States, especially the offshore islands of New York and Massachusetts. Cases have also been reported in Wisconsin, California, Georgia, and in some European countries.
Babesiosis causes a disease very similar to Malaria. Infection with Babesia parasites can be asymptomatic or cause a mild non-specific illness, and therefore many cases go unnoticed. In mild cases, people may experience mild fevers and anaemia. In more severe cases, fevers go up to 105°F / 40°C with shaking chills, and anaemia (haemolytic anaemia) can become severe. Organ failure may follow including adult respiratory distress syndrome.
In animals, there are a number of Babesia species which cause disease. Babesia canis rossi causes canine babesiosis and is vectored by the brown dog tick (Rhipicephalus sanguineus). This tick will feed on a wide variety of mammals, but dogs are the preferred host in the United States and appear to be required to develop large infestations. Canine babesiosis symptoms include fever, anorexia and anaemia.
Out of at least six Babesia species that have a considerable impact on livestock health and productivity, two species, Babesia bovis and Babesia bigemina have the greatest affect. Both of these piroplasms cause bovine babesiosis (tick-fever or cattle-fever) in cattle, economically the most important tick-borne disease of cattle worldwide.
Babesia bigemina is transmitted by Boophilus ticks while Babesia bovis is vectored by ticks of the genera Boophilus, Rhipicephalus, and Ixodes. Particularly severe forms of this disease can include a severe haemolytic anaemia.
B. bigemina is distributed wherever Boophilus ticks are encountered, which includes North and South America, Southern Europe, Africa, Asia and Australia. No vaccine against babesiosis is available.
Tick-borne Encephalitis (TBE)
Tick-borne encephalitis (TBE) or tick-borne meningoencephalitis (FSME) is a tick-borne viral infection of the central nervous system affecting humans as well as most other mammals. Caused by a member of the genus Flavivirus, the tick-borne encephalitis virus (TBEV) which has two subtypes; the European subtype, vectored by the sheep tick (Ixodes ricinus) and the Far Eastern subtype (Russian spring-summer encephalitis virus (RSSEV)), vectored by the taiga tick (I. persulcatus).The ticks act as both the vector and reservoir for the TBEV. The main hosts are small rodents, with humans being accidental hosts. Large animals are feeding hosts for the ticks, but do not play a role in maintenance of the virus. The virus can chronically infect ticks and is transmitted both transtadially (from larva to nymph to adult ticks) and transovarially (from adult female tick through eggs).
The virus can infect the brain (encephalitis), the membrane that surrounds the brain and spinal cord (meningitis) or both (meningoencephalitis). The disease is incurable once manifested, but infection can be prevented by vaccination, and the virus can be inactivated, halting disease progression. In humans the disease can be fatal. Person-to-person transmission has not been reported although vertical transmission from an infected mother to foetus has occurred.
TBE is an important infectious disease in many parts of Europe, the former Soviet Union, and Asia, corresponding to the distribution of the ixodid tick reservoir.
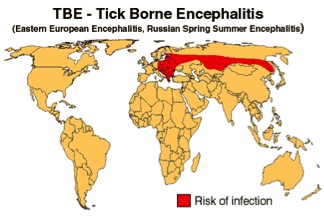
http://www.traveldoctor.info/diseases/10.html
Tularemia
Tularemia (also known as "rabbit fever" and "deer fly fever") is a disease that was first recognized as a plague-like disease of rodents in 1911 in Tulare, California. It is caused by a highly infectious bacterium (Francisella tularensis) that is widespread "in nature”, occurring in a variety of wild animals, in water, and even in soil. The bacterium is not dependent on arthropod transmission, but can be transmitted by the lone star tick (Amblyomma americanum) and also from deer flies. This disease has a worldwide distribution, but exists primarily in the northern hemisphere, including Asia and North America. Most cases occur in the south central United States.General symptoms include fever, headache, chills, nausea, and dry cough. An ulcerated lesion at the site of the bacteria inoculation (e.g. a tick bite) occurs in about 80% of patients. There is no vaccine for the general public, but one is available for people in high-risk occupations.

Tularemia lesion ex http://terrorisminfo.ucsf.edu/images/Tularemia-1.jpg

